Addicted to Fentanyl? Effective Help is Here
Fentanyl belongs to the class of opioid drugs, a synthetic administered according to a doctor’s prescription for severe pain, injury, or post-surgical pain treatment. However, it’s typically reserved for cancer patients, because it acts swiftly and eliminates the impression of pain.
However, many people misuse fentanyl because it produces such a powerful high for them. Because fentanyl is so much more powerful than morphine, this poses a number of serious risks. It has also increased the number of people who require effective fentanyl addiction treatment.
Keep reading to find out more about the addictive effects of fentanyl and how to get relief from the symptoms of fentanyl withdrawal at Catalina Behavioral Health!
Licensed Drug Addiction Treatment
The Power of Fentanyl
Doctors give fentanyl as patches, lollipops, a dissolving tongue film and dissolving tablets. There’s even a fentanyl nasal spray that was developed specifically for cancer patients undergoing radiation and other cancer treatment. In addition, fentanyl is given to surgical patients undergoing life altering procedures to relieve severe pain.
Fentanyl addiction is common even among people who take the drug as prescribed. Even without intentional drug abuse, the risk of fentanyl overdose is very real, regardless of who is using the drug.
Potent Prescription Drugs Hit the Streets
Street sellers or wholesale distributors blend fentanyl with cocaine, heroin, and other substances for an intense, more addictive high. Some people actively seek the substance out for its effects, while being aware of the dangers of fentanyl overdose and fentanyl addiction.
Many health problems can arise from fentanyl usage or overuse, especially when it is mixed with other medications.
In reality, fentanyl addiction is a serious problem. Tolerance and dependence on fentanyl hover heavily over anyone misusing the medication, even while utilizing the prescription according to the doctor’s directions. Once tolerance builds up, you need more and more of the medicine with each dose to feel its effects. When you no longer have a supply of the drug on hand, you begin experiencing what’s known as fentanyl withdrawal.
This is one of the worst forms of withdrawal in those with substance use disorder, and one that often calls for fentanyl addiction treatment options.
The Realities of Fentanyl Addiction

Opioids have risen to prominence as a source of fentanyl addiction and fatal overdoses due to widespread substance use disorders.
Fentanyl is widely used and is one of the most widely distributed synthetic opioids. Synthetic opioids like fentanyl became more frequently implicated in overdose deaths in the United States in 2016, surpassing prescription opioids – and steadily climbed from that point each year.
According to statistics compiled by the Centers for Disease Control and Prevention, the overdose deaths associated with these medicines climbed by a staggering 1,125% between 2011 and 2017. In spite of the fact that the opioid and fentanyl crisis is a countrywide problem, certain regions of the country were hit far worse than others as fentanyl addiction reached peak highs.
In fact, in 2017, 1,300 people in North Carolina died from overdoses using fentanyl and other synthetic opioids. That implies that out of the roughly 28,000 overdose deaths that happened nationwide, over 22% of them came only from North Carolina.
But now – fentanyl addiction has crept into every corner of the United States, with no state, city, or town, unaffected by the damage left in its wake.
The official numbers for 2021 were 107,622 overdose deaths total, with 71,238 of those attributed to fentanyl. This was a total increase of 15% – up from the total of 93,655 deaths in 2020.
What are Common Methods of Fentanyl Abuse?
Numerous preparations of fentanyl are available, including powder, drops on blotter paper resembling little candies, eye droppers, nasal sprays, and tablets that mimic legitimate opioid prescription medications. For this reason, fentanyl poses a significant threat. Some users who are consuming the substance aren’t even aware they are doing so.
It is possible that people will take what they believe to be a conventional opioid, but is actually fentanyl. It’s commonly mixed into batches of heroin because of the relatively low cost of fentanyl on the wholesale drug market.
Fentanyl comes in a wide variety of preparations and goes by a variety of names. Included on that list are Actiq, Subsys, Abstral, and Laszanda. Regardless of the branding, fentanyl abuse causes a variety of physical and mental effects.
The Negative Effects of Fentanyl Addiction
Fentanyl addiction can cause mental and physical impairments such as disorientation, sadness, trouble walking, slurred speech, muscular stiffness, a slower heart rate, hard breathing, and weakness. You’re also feel itchy and nauseous or dizzy and shaky. You might endure vomiting, weight loss, visual hallucinations, and pinpoint pupils as well. Abuse of fentanyl also carries the danger of sedation, respiratory depression, and ultimately death.
Fentanyl addiction treatment is an integral part of any successful rehab program. Psychotherapy gives the chance for sustainable recovery via your comprehension of why you abuse fentanyl in the first place. When you treat fentanyl addiction, it helps you understand what triggers you to engage in your substance use disorder, helping to prevent future abuse.
Long Term Effects of an Opioid Substance Use Disorder
Over time, fentanyl abuse causes a variety of undesirable outcomes. These go beyond the obvious signs and symptoms of drug usage and encompass both the mind and the body.
Fentanyl addiction can cause serious digestive issues such as constipation, intestinal blockage, and ripping of the colon. Additionally, your immune system declines, leaving you more susceptible to illness and infection. There’s also a marked personality change during active fentanyl abuse.
Combining fentanyl with other drugs, including heroin and cocaine, makes drug misuse more deadly. Using heroin or any depressant increases your risk of experiencing an overdose.
Combatting Fentanyl Withdrawal Symptoms

The only avenue to sustained recovery is fentanyl addiction treatment. Rehab, for instance, comes as the next logical step following detoxification and fentanyl withdrawal. Withdrawal produces several undesirable side effects of its own, although they feel far more manageable at during fentanyl addiction treatment. The severe symptoms of fentanyl withdrawal can be avoided, and the risk of recurrence can be mitigated, with medical monitoring throughout detox.
Chills, disorientation, weakness, diarrhea, joint and muscle pain, irritability, stomach cramps, trembling, tremors, restlessness, and loss of appetite are among fentanyl withdrawal symptoms. Detox is the first step on the road to recovery, but it’s only the beginning; the next step is receiving the necessary therapies during fentanyl addiction treatment. You have a considerably greater chance of relapsing and, as a result, of a fatal overdose if you don’t seek fentanyl addiction treatment.
How Does Addiction Treatment Help?
Fentanyl addiction, like any other opioid addiction, is battled via detox and addiction treatment. Detoxification from heroin, like that from any other drug, should only be attempted under medical supervision. Self-detoxing, also known as detoxing at home, is dangerous and should only be attempted with medical professionals present.
Counseling is employed in the treatment process to retrain the brain so that the individual no longer feels the need to use drugs or alcohol. The client’s drug-use expectations and behaviors can be modified with the aid of cognitive behavioral therapy, and stress and triggers can be better managed.
It’s possible that very low amounts of medicine might be utilized. Substitutes for fentanyl that bind to the same opioid receptors in the brain, such as buprenorphine and methadone, are effective in alleviating withdrawal symptoms. Naltrexone inhibits fentanyl’s effects by blocking opioid receptors. If your treatment provider thinks this will aid in your rehabilitation, they will likely suggest you try it.
24 Hour Fentanyl Addiction Hotline – Call Now!
What to Expect at a Fentanyl Treatment Center
An important first step toward a brighter future is the decision to stop taking drugs. When it comes to fentanyl, a fentanyl addiction treatment program may be your last opportunity for a normal future.
Consider your goals for therapy in order to choose an appropriate rehabilitation center. Addiction therapy is essential for those who abuse fentanyl-laced heroin, cocaine, painkillers, or even fentanyl on purpose. In these programs, you require numerous forms of treatment to get the most thorough recovery from your addiction.
Quality addiction treatment program aid comes from a high-quality rehab clinic. Furthermore, certification is crucial. This demonstrates the efficacy of the program for its participants. Accreditation also guarantees the rehab delivers the best quality programs, facilities, employees, treatment methods, and more.
What is a Dual Diagnosis Addiction Treatment Program?

Many people start misusing drugs or alcohol because they suffer from mental illness, such as depression, anxiety, or PTSD. Many mental diseases occur, thus they require expert diagnosis by a psychiatrist or other medical practitioner. Two or more mental health disorders are considered a “dual diagnosis.”
A primary prerequisite is the existence of addiction. There’s also the underlying mental disorder that served as a catalyst for your drug usage. Self-medication using drugs or alcohol regularly happens, even when you don’t recognize it.
Substance misuse can also lead to mental health problems for certain people. However, it does not matter which of your co-occurring disorders originated first. What counts is the means by which you acquire therapy, with both being dependent on it simultaneously. Both of your illnesses will recur if you neglect to treat either one of them.
Detoxification from Fentanyl and Medication-Assisted Therapy
Medically assisted fentanyl detox allows clients to be weaned off the drug gradually or to be treated and/or maintained by drugs throughout withdrawal. Those struggling with fentanyl addiction, however, will need to attend rehabilitation after detoxing.
The withdrawal from fentanyl can cause a wide variety of symptoms. This condition is exceedingly acute and can be very unpleasant, painful, even hazardous. Fentanyl is a powerful opioid, and its withdrawal symptoms prompt many former users to return to drug abuse. Some of the possible symptoms are:
- Watery eyes and runny nose
- Anxiety
- Irritability
- Discomfort
- Goosebumps on the skin, chills, or sweating
- Stomach pain
- Intestinal distress, nausea, and/or vomiting
It is common for fentanyl addicts to have severe pain in their muscles, joints, and bones when they go through withdrawal. Some people may also have severe psychological symptoms, such as panic, sadness, or irritability.
At any time, these symptoms may become quite severe. Medical supervision in a detox center or drug treatment facility can make the process of withdrawal from fentanyl far more tolerable and less harmful.
The Benefits of Medication Assisted Treatment
Stabilizing drugs can be given to people in detox to lessen the intensity of withdrawal. Opioid detoxification drugs include methadone, buprenorphine, and Naltrexone.
- Having effective medical help
- Nursing care is available around the clock
- Medication can help alleviate some of the discomfort
- In addition to education, you also have access to peer support for your addiction.
- The counseling and therapy services available to you.
- A plan for your care following hospital discharge will be made, and you will get follow-up treatment.
- You’ll develop relapse prevention techniques.
Finding a detox center or drug treatment facility that provides medically assisted detox is essential if you want to get help for your fentanyl addiction. This will guarantee you have the safest and most comfortable detox experience possible, and it will also give you access to ongoing addiction treatment programs so you can achieve long-term sobriety. However, it should be mentioned, the stabilizing procedure may take up to a few weeks.
Difficulties of Treating Fentanyl Dependence with Buprenorphine
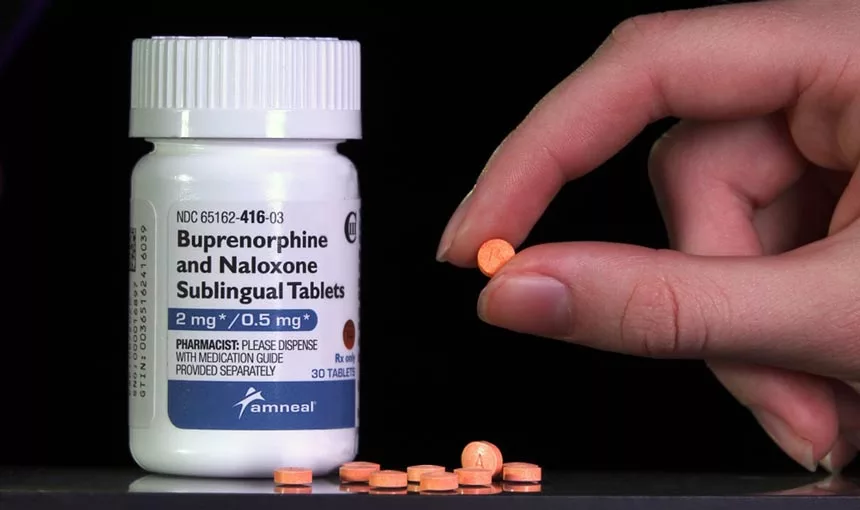
While clinicians across the U.S. and Canada, where fentanyl is also common, have observed that buprenorphine inductions have gotten more difficult in recent years, the phenomenon is impossible to assess or explain. Theories include fentanyl’s sheer power, or because it is lipophilic — it adheres to fat molecules — and lingers in the bloodstream for longer than other opioids.
Buprenorphine is what’s known as a partial agonist, meaning that it binds firmly but incompletely to the same brain receptors that generate a euphoric sensation when opioids attach to them. It attaches to the receptor, but it does so awkwardly, like a piece of a jigsaw that doesn’t quite fit. Addiction medicine can displace fentanyl in the body, causing the client to experience “precipitated withdrawal” if they are already dependent on opioids.
As a result, it’s conmon for doctors to wait several hours until clients start suffering withdrawal symptoms before they prescribe buprenorphine. At that moment, the “bupe,” as it is known, helps to relieve withdrawal symptoms like anxiety or gastrointestinal distress, as well as reduce future opiate cravings.
Failed Induction and Opioid Receptors in the Brain
With fentanyl, however, doctors are frequently obliged to wait a full day, if not longer, to be sure buprenorphine doesn’t induce extreme agony. In other circumstances, even individuals experiencing withdrawal because they refrained from drug use for several hours — generally excellent candidates for buprenorphine — discover that their symptoms grow worse, not better, after they begin using the prescription. Many don’t return back for another dosage, described in doctors’ lingo as a “failed induction.”
Doctors say that unsuccessful attempts can be perilous — not simply because they risk patients relapsing to fentanyl use, but also because those patients can feel so bad that they refuse to ever try buprenorphine again.
Clients are increasingly asking for methadone, despite the fact that it has a number of drawbacks, according to some medical professionals.
Despite the pervasive nature of this issue, medical professionals have yet to agree on a course of action. Doctors have to rely on unofficial sources like word of mouth and newly published scientific articles because they haven’t gotten much formal direction from medical associations or local health officials.
24 Hour Addiction Treatment – Get Help Now
Different Attempts at Introduction
In the interim, though, doctors are utilizing techniques that differ widely. In an effort to overcome withdrawal symptoms more forcefully, some have began providing much higher quantities of buprenorphine, sometimes as much as 32 milligrams, or four times the customary initial dosage.
Some physicians employ ordinary pharmaceuticals to address any leftover feelings of physical discomfort and anxiety, including antihistamines, ibuprofen, and pills to battle nausea and gastrointestinal disorders.
Others have attempted “microdosing,” in which buprenorphine is gradually increased over the course of several days to prevent withdrawal symptoms from occurring all at once. Some doctors have administered shorter-acting opioids generally used for pain, such as hydromorphone, to reduce withdrawal symptoms while clients build up to bigger doses of buprenorphine over the course of days or weeks.
Treating Severe Pain and Withdrawal with Medical Supervision
Others, still, have tried the controversial technique of providing naloxone, a medicine intended to counteract opioid overdoses, even to clients who are not overdosing. This results in a brief period of acute withdrawal that prepares the client for a first dosage of buprenorphine that reduces rather than increases pain.
Any method that succeeds is encouraging. However, it is worrying that it is becoming more difficult for doctors to prescribe buprenorphine. Despite the drug’s obvious benefits, it has historically been difficult to persuade primary care physicians or other non-addiction experts to prescribe it. Some doctors are concerned these new challenges may undo the progress previously made in fentanyl abuse treatment.
Effective Measures for Opioid Withdrawal Symptoms
Still, some physicians remain optimistic. And clients who wish to begin buprenorphine therapy shouldn’t stress too much. Ultimately, buprenorphine introduction for those taking fentanyl is still achievable, despite its obstacles.
The regularity and potency of fentanyl in the North American drug market do make the induction a bit more challenging. However, with one of the unorthodox induction methods mentioned above, introducing the drug can still happen with limited pain and efficient results.
What Preparations Must Be Made Prior to Fentanyl Rehab?
It’s important to study as much as possible about fentanyl detox and rehab before you begin the program. Before your first detox visit, you may have questions like:
- What the rules are regarding items you can and can’t bring
- How long is the entire process of detox and and rehab combined
- How intense will withdrawal symptoms be during detox?
- What methods are used to increase my comfort?
- If I do require medicine, what exactly do I need to take?
- What are the meal plans?
- Can I have a phone or can family visit?
If you know what to expect during detox, you may prepare yourself mentally and set reasonable expectations for yourself.
Specific Types of Therapy Offered During Treatment

- Cognitive-behavioral treatment
- Dialectical behavior treatment
- Holistic treatment
- Group therapy
- Family therapy
These take place within one of the following levels of care:
Inpatient
You live at the facility and have 24-hour access to medical professionals in addition to counselors, and participate in group therapy.
Outpatient
Less intense form of treatment that allows you to reside at home. You’re still required to attend a facility for rehab for a certain number of hours each week – typically two days for 2-3 hours each day.
Intensive Outpatient Program
Intensive outpatient follows the same protocols as standard outpatient, but your participation time is increased to a minimum of 9-12 hours per week instead of 4-6.
Partial Hospitalization
This is the most intense besides inpatient. In a partial hospitalization setting you are allowed to live at home – however, you’re normally required to remain at the facility for the duration of the day – normally, 8-10 hours.
Immediate Placement for Addiction Treatment
Catalina Behavioral Health Offers These Options and More
If you or someone you know is suffering from fentanyl dependence, you don’t have to continue to fight the battle alone. At Catalina Behavioral, we understand that fighting substance use is one of the most difficult battles you’ll ever face throughout your entire life.
Failure to have a proper support structure and recovery team, unfortunately, leaves you in a revolving state of recovery and relapse. To obtain the treatment you need, contact Catalina Behavioral Health and speak with our admissions team today!





