The Importance of Detox for Substance Abuse
Medical detoxification refers to the removal of drugs or alcohol from a client’s physical system. Its purpose is to assist patients in overcoming physical dependence by mitigating withdrawal symptoms experienced.
Substance addiction withdrawal can be fatal in extreme cases. Medical personnel can properly treat the symptoms of withdrawal by administering medicines and other procedures in controlled settings such as detox facilities and addiction rehabilitation centers.
Everyone responds differently to withdrawal. Medical detox plans vary in length, intensity, and pharmaceutical approach depending on the nature of the addiction, the client’s background, and the facility’s capacity to treat it.
Always keep in mind that the underlying behavioral, environmental, and genetic factors of addiction are not addressed by medical detoxification. Education, counseling, and other long-term support services should follow as the next steps in addiction treatment.
Keep reading to find out more about medical detox at Catalina Behavioral, and how their program makes detox as effective and comfortable as possible!
Safe and Comfortable Detox Setting – Call Now!
Who Benefits from a Medical Detox Program?
The human body develops a drug abuse issue or addiction when the presence of alcohol or other substances begins to control the mind and body after prolonged use. The brain eventually adjusts to the drug’s effects and resumes regular functioning. A person’s tolerance to medication increases with time, necessitating increasingly large dosages to get the same benefits.
Eventually, the body develops a tolerance to the alcohol or substance use and becomes dependent on it for regular functioning. When a person stops taking a drug, their body responds unfavorably, and they may experience withdrawal symptoms such as headaches, fever, vomiting, and other unpleasant physical and mental impacts. When the body isn’t given the medications it’s craving, potentially life-threatening detox symptoms could prevail.
Overcoming Withdrawal Symptoms

Those trying to stop drinking or using drugs face significant challenges, including intense cravings and uncomfortable withdrawal side effects. Fortunately, medical detox under supervision can help people safely go through withdrawal. Eventually, the body learns how to operate normally again without the medication, and the cravings go away – especially after a significant period of substance abuse treatment.
Medication and monitoring can be provided on an outpatient basis for less serious conditions. A person with a serious addiction to drugs or alcohol should seek treatment at an inpatient center or drug rehab facility, where they can undergo supervised medical detoxification.
The following substance all potentially require the need for medical detox:
- Alcohol
- Opioids
- Benzodiazepines
- Meth
- Cocaine
- Prescription medications
- Synthetic or Designer Drugs (such as Spice, K2, and bath salts)
How Does Medical Detox Work for Drug Abuse?
Medical detox at a treatment center involves three main phases: assessment, stabilization, and treatment planning. Clients in medical detox may also participate in education programs, counseling, and support group meetings for addiction recovery.
Evaluation of Substance Use
A questionnaire, physical exam, blood tests, and screening for co-occurring mental health problems or other medical diseases are the normal components of an evaluation. During an evaluation, therapists will determine how mentally stable a patient is and how solid their support system is.
The results of the examination will be used by the doctor to formulate a treatment strategy. You should only begin this process if you’re serious about medical detox – it’s not intended to be professional medical advice – it’s the entry stage to inpatient detox.
Stabilization and Care Planning
The stabilization phase involves the client discontinuing drug or alcohol use with the assistance of medical specialists in order to attain sobriety and physical stability. There are medications that can help with the discomfort of detoxing from particular substances, such as alcohol, nicotine, and opioids.
Depending upon the degree and kind of addiction, the duration and intensity of withdrawal symptoms vary. Stabilization normally lasts between one and three weeks. Clonidine-assisted heroin detoxification has been known to provide substantial relief from painful side effects during medical detox.
Preparation for the Next Steps
Clients should be prepared for continued individual and group therapy following medical detox. While medical detox helps alleviate some of the most unpleasant physical symptoms of recovery, it offers nothing to help patients cope with the psychological obstacles they’ll confront in the days and weeks that follow. Therapists, 12-step facilitators, and other medical experts should stress to their clients the value of starting long-term treatment as soon as possible.
Medical Detox Hotline – Immediate Help
Exit Strategies and Detoxification Types
The majority of healthcare professionals, public health officials, and addiction experts favor the medical approach of detoxification. The medical model, which includes nursing staff, medicine, and physician monitoring throughout the process, forms the foundation of the Substance Abuse and Mental Health Services Administration’s principles of effective detox.
- Among the many methods used to treat addiction, detoxification is just one.
- Detox involves assessment, stabilization, and treatment preparation.
- Regardless of the severity of their illness, everyone should follow through with the entire process.
- Customized detox programs are the best option.
- All clients should be sent to treatment following detox.
- The complete process of medical detox has to be covered by medical insurance.
- Future therapy compliance and client engagement are indicative of a successful outcome.
Medication or medical treatment is not part of the social model of detoxification. It is based on the idea that people may be helped through withdrawal with little TLC and a positive support system. Twelve-step programs and other types of support groups are good examples.
Sober Support Systems Following Detox

These days, it’s common for centers that treat substance abuse and alcohol abuse to include both medical and social approaches. While getting professional medical care, clients at these centers have the option to participate in 12-step programs like Alcoholics Anonymous and Narcotics Anonymous, as well as SMART Recovery.
No matter what kind of detox program is being used, SAMHSA has established certain universal standards for success. Even for detox from ketamine and similar drugs, where the symptoms are largely psychological, a medical setting is advised for the following reasons:
- In accordance with these rules, teach the person how to withdraw safely.
- Engage support networks such as friends, family members, and peer groups.
- Preserve an alcohol- and drug-free atmosphere.
- Improve your motivation by using the methods provided.
- Cultivate a connection with the client that can lead to therapeutic change.
Both the social and the medical detox models share a focus on the client’s well-being and safety during the process. Unfortunately, not all methods are harmless, no matter how well-meaning their proponents may be.
The Risks of “Cold Turkey” Detox
Many people who struggle with alcohol or drug addiction try to kick the habit by “going cold turkey.” When someone is physically or psychologically reliant on a substance, the cold-turkey method might be fatal.
Attempting to stop without first gradually reducing intake (known as “tapering”) is associated with more painful withdrawal symptoms. A fatal overdose can occur during the withdrawal process for people with serious addictions to alcohol or benzodiazepines.
Accelerated Detoxification: A Risky Proposition
Ultra-rapid detox methods were created in the early 1990s to help heroin and opiate addicts cope with withdrawal. Ultra-rapid detox, however, has been shown in a number of studies to not only not reduce withdrawal but also to pose significant hazards to patients.
During ultra-rapid detox, patients are sedated and then given a drug that accelerates the withdrawal process. Patients were expected to rest through the most uncomfortable periods of withdrawal.
However, research shows that individuals who received the medication still had withdrawal symptoms upon waking. Unfortunately, the procedure was not sped up by this approach, and patients with preexisting medical illnesses, including diabetes, heart disease, HIV/AIDS, or co-occurring mental health issues, were at risk for consequences.
Medication Assisted Treatment and Medical Detox
Medication-assisted therapy aims to alleviate symptoms and restore health by eliminating the need for the client to deal with withdrawal. The procedure is supervised by a doctor or a team of medical professionals, such as nurses or other specialists in mental health.
The majority of drugs used to treat withdrawal symptoms focus on alleviating physical symptoms like aches and pains, nausea and vomiting, and sometimes even seizures and tremors. Unfortunately, there is no prescription that will speed up the body’s natural detoxification processes, although there are several that can help with cravings.
The following substances are used throughout the detox process:
Benzodiazepines and the Risk of Seizures
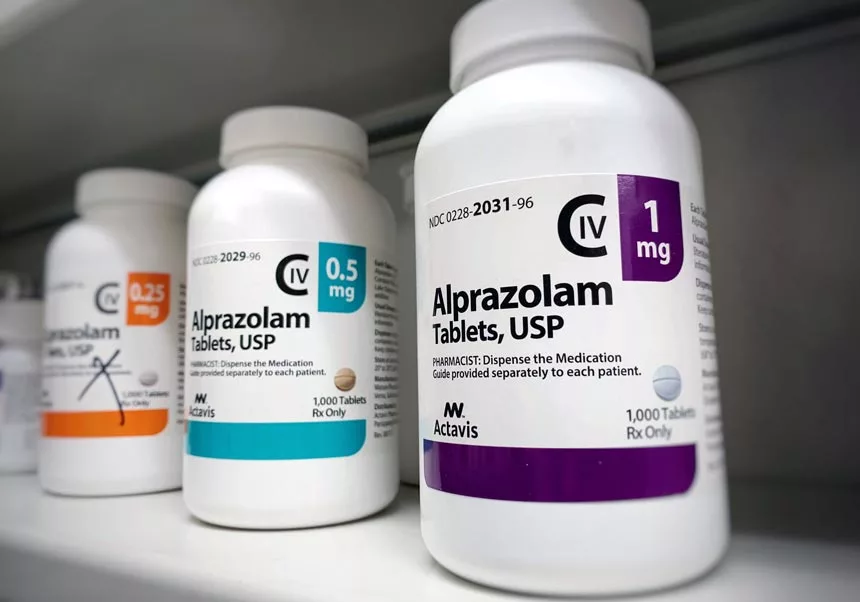
Benzodiazepines are prescribed by doctors for the treatment of anxiety, insomnia, and alcohol withdrawal. Although benzos are the medicine of choice for alcohol detox, their significant misuse potential means they are often exclusively used in inpatient institutions rather than outpatient clinics.
The medication reduces shaking and nervousness and lessens the likelihood of having a seizure or delirium.
Detoxification benzodiazepines include, among others, Librium (chlordiazepoxide), Valium (diazepam), Ativan (lorazepam), Serax (oxazepam), and Klonopin (clonazepam).
During medical detox at benzo rehabs Arizona, and elsewhere, doctors often administer long-acting benzodiazepines like Valium, but patients with liver issues may benefit more from short-acting medicines like Ativan or Serax.
The medications can also be used to lessen the effects of anxiety brought on by hallucinogens like LSD. Patients will be weaned off benzodiazepines gradually over the course of several days once they have stabilized. Suddenly, withdrawal symptoms from stopping a high dose of benzodiazepines might be severe in itself.
Anticonvulsants as Taper Medications
Anticonvulsants are used to prevent or lower the risk of seizures, especially in the case of alcohol addiction. You’ll often see them employed in the context of benzodiazepine and alcohol withdrawal. There is evidence that anticonvulsants are effective at regulating mood in people with bipolar illness.
Atretol (esketamine), Neurontin (gabapentin), and Trileptal (oxcarbazepine) are a few of the anticonvulsants that may be prescribed during detox.
Women who are pregnant and going through detox should be informed of the link between anticonvulsants and birth defects.
Antipsychotics in Medical Detox Settings
Addiction experts utilize antipsychotics to treat agitation, delusions, hallucinations, and delirium during medically supervised detox. Even though they can raise the risk of seizure in some people, they are frequently used to treat psychotic symptoms in patients with co-occurring mental health conditions.
While antipsychotics are often used during alcohol detox, they are seldom utilized to manage hallucinogen-induced psychosis. When it comes to antipsychotics, Haldol (haloperidol) is among the most often utilized. Most facilities avoid older antipsychotics like Thorazine (chlorpromazine) because of the risk they pose to patients by lowering their seizure threshold.
Antidepressants in Dual Diagnosis Cases

Co-occurring mental health illnesses are frequent, and antidepressants are often recommended to treat them; however, these medications can have undesirable side effects, including sleepiness, high blood pressure, and even loss of consciousness.
Anxiety, sleepiness, and sleeplessness have been linked to selective serotonin reuptake inhibitors, a relatively new family of antidepressants. As an added downside, users who suddenly cut back on their drug use may experience withdrawal symptoms.
However, for individuals with clinical depression or suicidal ideation, the medications can be helpful. Many people choose SSRIs since they produce fewer adverse effects and don’t interact badly with other medications.
Clients detoxing from amphetamines or hallucinogens are more likely to obtain antidepressants than those detoxing from other substances because they commonly feel depression during withdrawal.
Insomnia during detox is sometimes treated with sedative antidepressants like Oleptro (trazodone) or Tofranil (imipramine). Because of the potential for increased seizure risk, their usage requires caution.
Clonidine and Blood Pressure in Detox
Clonidine, a blood pressure medication, is sometimes recommended to individuals undergoing multiple drug detoxification. Clonidine can lessen the severity of alcohol withdrawal symptoms in those who have heart disease or high blood pressure. However, it does not lessen the possibility of a seizure or delirium.
Though clonidine may help alleviate certain withdrawal symptoms from opioids, it’s usually combined with other drugs because it isn’t as effective as methadone or buprenorphine on its own.
Methadone as a MAT Option
It’s important to note that methadone is a prescribed opioid. Among medications used for opioid withdrawal, it is by far the most popular. Those seeking to detox from opioids can only get a prescription for methadone from a clinic that has been approved by the government. The medication reduces cravings and other withdrawal symptoms, typically on an outpatient treatment basis.
Methadone is also highly addictive, and misuse can lead to physical dependence, psychological dependence, and even death. This is why there are so many rules surrounding the usage of methadone in detox.
To begin methadone detox, a qualified medical professional will determine the optimal methadone dosage to minimize withdrawal symptoms. After then, the dosage is gradually decreased over the course of three to five days, usually by 5 or 10 milligrams each day. Patients with more severe addictions may require methadone maintenance therapy, which is a long-term treatment for addiction, but not an option offered at Catalina Behavioral Health.
24 Hour Addiction Treatment – Get Help Now
Buprenorphine (Suboxone as MAT Medication)
Buprenorphine is a relatively new medicine that many experts feel can successfully replace methadone in the treatment of opioid withdrawal. Buprenex, an injectable form of buprenorphine, has been authorized by the FDA for use in opioid detox. Other versions of buprenorphine, such as Subutex and Suboxone, are licensed for addiction treatment but are not recommended for usage during detox, but more often as a part of an inpatient or outpatient program following detox from opiates.
Buprenorphine is significantly safer than methadone and effective in alleviating withdrawal symptoms. On the other hand, it has little possibility of inducing euphoria or suppressing breathing. Certified doctors can prescribe can also provide medication assisted treatment for outpatient detox.
Additional Options for MAT in Detox

Patients may encounter a broad assortment of withdrawal symptoms during detox. Medication is commonly prescribed by doctors to manage withdrawal symptoms when they arise.
Common medicines or supplements used during detox include:
- Anti-nausea medicine, such as Zofran (ondansetron) or Pepto-Bismol (bismuth subsalicylate)
- Options to relieve pain and lower temperature, such as acetaminophen (Tylenol), ibuprofen (Advil), or aspirin
- Sedatives, such as Benadryl (diphenhydramine) or Vistaril (hydroxyzine)
- Fiber pills, milk of magnesia, and other laxatives are available.
In an effort to alleviate their patients’ discomfort, medical staff must balance the risks of adverse drug reactions with the benefits of giving patients the pharmaceuticals they need.
Preparing for Medical Detoxification
The procedure begins with an evaluation. The severity of a patient’s disease, as well as their medical history and any drug or alcohol misuse, will be factors in the questions asked by doctors. They’ll assess individuals for co-occurring mental health issues, infectious diseases, and nutritional deficits. Patients are often screened for things like TB, dental health, and trauma.
A physician or addiction expert will gather patient information and formulate a strategy to ensure the client’s health and well-being. Clients receiving care in inpatient facilities will be given a private room and closely watched around the clock for roughly a week. Appointment plans and schedules are often made by doctors or therapists in outpatient clinics.
A detox may be uncomfortable, even with medical assistance. After it’s done, patients are in better condition and can concentrate on the next step of their treatment.
The two most common reasons for medical detox – alcohol and opioids, entail different steps to overcome each. Below, we outline the detox process for both.
Acute Alcohol Withdrawal
Detoxing requires close medical care for those with moderate to severe alcohol dependency. Alcohol withdrawal symptoms can start while there is still alcohol in the blood, although they often appear between six and twenty-four hours after the last drink.
Symptoms include:
- Anxiety
- Fever
- Nausea
- Vomiting
- Insomnia
- Hallucinations
- Delusions
- Seizures
Without medical care, alcohol withdrawal may be lethal. It can lead to potentially fatal blood pressure, heart rate, and temperature elevations. Death can also be the result of delirium tremens or seizures.
In a drug-free alcohol detox program, patients will be provided with one-on-one care, as well as access to water and food. If you have a minor alcohol use disorder and have never gone through alcohol withdrawal before, you may find success with nonmedical methods, but it is best to consult a physician or our team for a confidential assessment of your needs.
Opioid Withdrawal Symptoms in Detox

Opioid withdrawal symptoms are unpleasant but seldom life-threatening. There is a lot of overlap between the withdrawal symptoms of pharmaceutical opioids like oxycodone, fentanyl, and codeine and illicit drugs like heroin. The intensity and duration of opioid withdrawal symptoms vary, depending on the substance in question.
Heroin withdrawal symptoms often appear between 8 and 12 hours after the last dosage, and detoxing from heroin addiction typically takes three to five days. Rapid deterioration into severe withdrawal symptoms begins about day two following the last dosage of methadone. It takes at least three weeks to detox from methadone use.
Opioid withdrawal causes the following symptoms:
- Racing heart
- Chronic hypertension
- Fever
- Insomnia
- Sweating
- Nausea
- Vomiting
- Pain in the Muscles
- Anxiety
Medication to alleviate withdrawal symptoms is recommended for people undergoing opioid detox. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), avoiding medically assisted detox can lead to needless suffering.
Detoxification from opioids may involve the use of medications such as:
- Methadone
- Buprenorphine
- Clonidine
- Sedatives
- Stomach medication
- Laxatives
Get Immediate Placement for Detox – Call Now!
Recover Without Painful Detox or Withdrawal Issues
At Catalina Behavioral Health, we know how frustrating the detox process can be. It’s difficult to say how much pain and discomfort you’ll experience – but we have a significant amount of experience in providing comfort to those who need it most during the withdrawal period.
Our goal is to provide all our clients with the most comfortable experience possible and, in the end, help guide them to long-term recovery.
For more information on our detox program, contact our admissions team today!







